SOB UNDER EVALUATION SECONDARY TO ? RIGHT HEART FAILURE
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment
A 16 year old male patient came to the OPD with chief complaints of
Swelling of both the ankles since 8 days
Headache since 4 days
Shortness Of Breath since 7 days
HISTORY OF PRESENTING ILLNESS:
The patient was apparently asymptomatic 8 days back, later he developed swelling of both lower limbs which was insidious in onset. Swelling of face was noted by his mother after playing. Later he was taken to a government hospital and he was tested for bilirubin levels and was diagnosed as Jaundice.
As per the history provided by the patient, on the next day, he came to our hospital as he noticed swelling, first in the face and then after a day, noticed in both the lower limbs and a day after, he noticed swelling of abdomen. He used dytor tablet (single) and came for admission after 2 days.
Shortness of breath on exertion since 7 days, episode lasts for 30mins and subsides after taking rest for few minutes and also at night
Dragging type and superficial pain of scalp since 4 days, continuous in nature for 2 days, later subsided
HISTORY OF PAST ILLNESS:
Not a K/C/O DM, HTN, Epilepsy, Asthma, COPD
H/O reccurent lesions and ulcers over the margins of tongue and inner margins of lips since 6 years for which he was given a mouth wash by a local doctor
Frequency : Weekly once since 6 years but now decreased in frequency and last ulcer appeared 2 months back
FAMILY HISTORY:
H/O Hypertension in the family (Grandmother since 5 years)
PERSONAL HISTORY:
Appetite - Normal
Sleep - Adequate
Bowel & Bladder - Regular
Micturition - Decreased urine output since 8 days
Diet - Mixed
Addictions - Occasional Toddy Drinker
GENERAL PHYSICAL EXAMINATION:
Patient is conscious, coherent and co-operative and well oriented to time, place & person
Pallor - Mild
No Icterus
No Cyanosis
No Clubbing
No Lymphadenopathy
Pedal Edema - Subsided
Slight brownish discoloration of hair seen since 3-4years
Vitals: - 110/70mmHg
PR - 97bpm
SpO2 - 98%@RA
Temperature - 98.5 °F
SYSTEMIC EXAMINATION:
RESPIRATORY SYSTEM:
BAE - present, NVBS heard
CARDIOVASCULAR SYSTEM:
S1, S2 heard, JVP raised, No murmurs
CENTRAL NERVOUS SYSTEM: NAD
CLINICAL IMAGES:
CHEST:
ABDOMEN:
EYES: Mild pallor
HAIR: Brownish-white discoloration seen
PROVISIONAL DIAGNOSIS: SOB UNDER EVALUATION
INVESTIGATIONS:
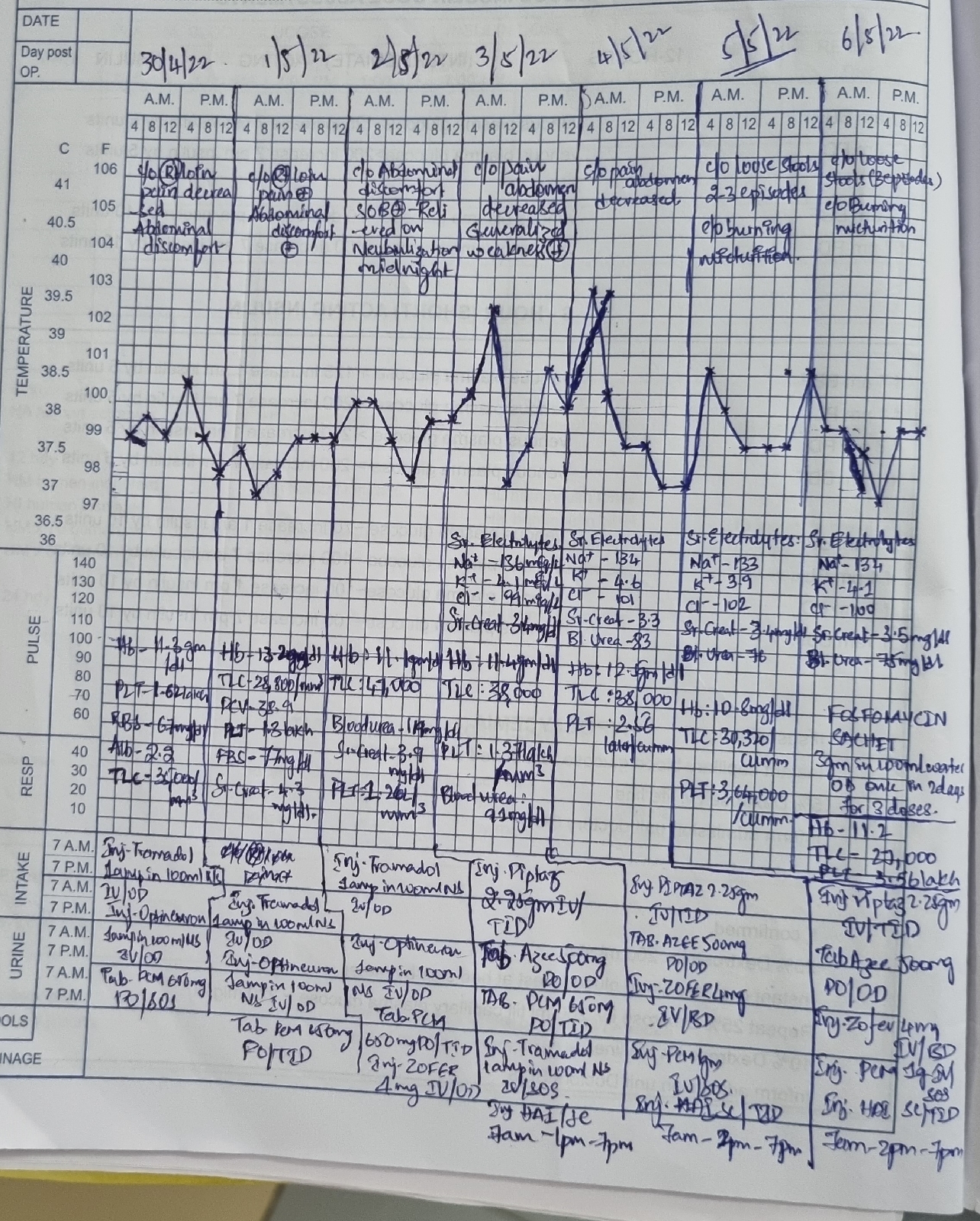
CBP:
LFT:
Serum Creatinine:
Serum Electrolytes:
Serum Uric Acid:
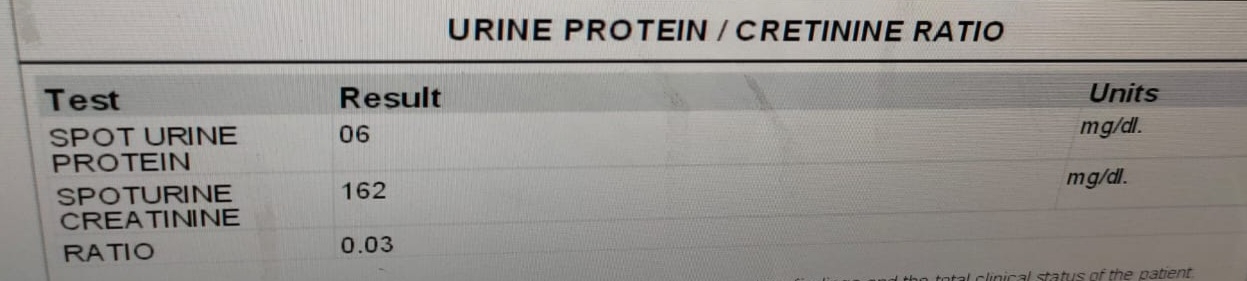
Spot Urine Protien/Creatinine Ratio:
ECG:
2D ECHO:
USG ABDOMEN: